 |
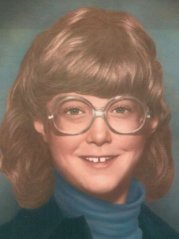
In The Palm of Her Hand – written by Julie’s Mother Julie Therese… a vibrant child who charmed everyone she met and dearly loved by her parents and two younger sisters…Karen, 8, and Meghan, 3. She seemed able to strike up a conversation with the oldest adult…and play on the level of the smallest child. |
I was Julie’s Girl Scout leader before Christmas in 1979 when our troop decorated a tree and sang carols for the residents at a local nursing home.
One of the residents told Julie it would be her first Christmas ever without her family.
And so, on that busy Christmas morning in the midst of toys, gifts and wrappings, it came as no surprise to me when she asked to bring flowers to her “new friend” at the nursing home…a gift for a special lady on Christmas Day from a very special nine year old girl.
It would be our last Christmas ever with Julie.
The winter of 1980 was uneventful for our family. I was oblivious to the fact that Reye’s Syndrome was devastating the lives of children and families all over the country. There were 548 cases of Reyes reported to the Center for Disease Control that year (113 in Ohio) with at least 107 deaths. Five deaths were reported in Ohio… But not in the news!
July of 1980 came and Julie spent her usual week at Girl Scout Camp. While she was away, several children in town became ill with what appeared to be “just cold” symptoms…sore throats, low-grade fever. The swim meet scheduled for Karen was cancelled since so many swimmers were down with “whatever was going around”. And then Meghan developed a sore throat and fever. Aspirin, one and ¼ grain (80 mg.) per year of age every four hours for fever over 101 degrees was the standard in 1980.
I gave Meghan two, chewable, orange flavored, Bayer Baby Aspirin. She recovered within 24 hours and Julie came home from camp. The following week Karen developed a fever of 102 degrees that remained elevated for a few days. On her birthday, July 25th, suspecting that it might be strep throat, I took her to our pediatrician for a throat culture which proved to be negative. “Just a simple viral infection”, I was told by the nurse on the phone. “Continue the aspirin and fluids and call if she is not better by Monday”. Karen, thankfully, recovered.
Years later I learned that it was July of 1980 when studies done in Arizona, Ohio and Michigan suggested a connection between the use of aspirin with the initial infection (flu, chicken pox) and the development of Reye’s Syndrome.
Julie was so active over the weekend catching up on her summer reading and swimming with her friends at the pool… I gave little thought to the fact that perhaps she would also catch this mysterious summer virus. But on Monday morning, July 28th, as we headed out for swim team practice, Julie asked me to drop her off at the library. “I don’t feel good and if I’m going to be sick, I want plenty of books to read.” Even now I am sickened by the thought of what happened next. I can see her standing in the kitchen while I placed one adult aspirin (325mg) and two “baby” aspirin in the palm of her hand.
Was it all a dream? No, it was a mother’s worse nightmare. I gave her a substance which would be toxic for her. It was the first day of the last week of my beautiful daughter’s life.
By Wednesday morning Julie had recovered and my thoughts turned to preparing for house guests scheduled to arrive late Thursday. Julie was very excited since she had not seen her friend Leah, since she had moved to Michigan. But something still wasn’t quite right with Julie. We went to MacDonald’s Wednesday evening and she said she didn’t feel like eating. No nausea or stomach pain; just no appetite.
No appetite for MacDonald’s? Surprised and feeling somewhat anxious, I brought her home and she went to bed before the sun went down.
Julie’s malaise continued through Thursday but she was up to greet Leah when the family arrived Thursday night. They trotted off together to the girl’s bedroom where we could hear the sounds of their chatter and laughter drifting through the house.
Thank God…she seems to be OK. You are definitely a nervous Mom. Just calm down.
Friday, August 1st. The girls were up bright and early making plans for the day. Julie, at last, ate a good breakfast of French toast; her favorite. I took the other children to the pool while Leah’s mom took Julie and Leah to the mall for haircuts…much to their delight!
Life had returned to normal… the weather was hot but it didn’t matter… I knew it was going to be a great weekend.
It was noon and I was in the driveway unloading wet suits, towels and pool toys when Leah came running out of the house. “Julie threw up in the beauty shop!” she yelled.
I found Julie in her room reading in bed. “Are you OK? What happened?” I asked. She explained that she “just threw up” on the floor. She didn’t know she was about to be sick and couldn’t make it to the restroom. Her tummy felt soft to touch. She did not complain of pain or cramping. No headache, but very thirsty. I brought her ice chips… and waited, almost prayerfully, for the diarrhea to begin.
Later, Leah’s mother said that Julie had vomited “suddenly and forcefully” at the mall. It continued that way for the next six hours, frequently and relentlessly, until the vomiting was reduced to nothing but dry heaves. At 8:00 P.M. I called our pediatrician at his home. He said it was most likely a severe gastroenteritis and warned that it would probably “go through the whole family”. And our house guests, too, I thought! “If she continues to vomit, bring her to the office in the morning”.
In retrospect, I wish he didn’t have Saturday morning office hours. If only we had just brought her directly to the emergency room. The first of a long list of “if only’s” had begun.
It was a long night. Julie climbed into bed with me. But she was restless and occasionally tip-toed to the kitchen for more ice. The vomiting appeared to have ended. At about 5:00 A.M., Saturday, she asked to go out to the couch in the family room. I followed and noticed that she seemed to stagger a little as she walked down the hallway.
Across the room, through the glass sliding doors, I watched a beautiful sunrise. When I called her attention to it, she looked at me groggily and in an irritable voice said, “I don’t want to look at the sunrise.” And then, “Mom, I want Leah to leave…”
Dear God…Something is terribly wrong with Julie, I prayed. This is not happening!
A few minutes after 6:00 A.M., I told Julie’s Dad “I’m worried. I’m taking her to see Dr. C. at nine o’clock.” Bill, always the optimist, reassured us that Julie would be just fine.
Of course, she’s going to be fine. She was sick to her stomach…probably something she ate. Dr. C. will wonder why you ever brought her in…
Julie was quiet on the way to see the doctor. She didn’t even want to bring along her book that she was reading from the Boxcar Children series. But she begged me for water. Certain now that the vomiting was over, I gave her a full glass. “Much better”, she smiled.
When we arrived at the doctor’s office, she threw up in the parking lot. Clear liquid. With difficulty, she walked into the doctor’s office.
For the first time, Reye’s Syndrome flashed through my mind. But I quickly put that one to rest. No…it’s summer. This cannot be the flu. And she had chicken pox in 1978…during the blizzard.
“Hello, Julie! Give me five!” Doctor C. said when he saw her. Julie responded with her good-natured high five. She knew that he would make her better. She loved Dr. C. and he had always made her feel better…usually within hours. He quickly began to examine her…no fever, abdomen soft and non-tender, neuro exam unremarkable. He looked at me and quietly stated “I know what you’re thinking, Mom. It is not Reye’s Syndrome!”
He couldn’t know what I was thinking…but now I knew what he was thinking. At the time, however, I did not know that a blood test for ammonia levels and liver function was available to help with a diagnosis. But he did. Strange, I thought…. he told me to call him at 6:00 P.M…one way or the other.
He sent us home with a prescription for a Tigan suppository…an antiemetic that would help her stop vomiting. The pharmacist seemed reluctant to give it to a child and called the doctor’s office to confirm his choice of medication.
At 12 noon, after a struggle to help Julie, now stumbling and holding onto the walls, I got her back to bed and gave her the suppository.
Again, I learned a few weeks later that the FDA had issued a warning that anti-nausea drugs such as Tigan should be avoided with vomiting in children since it may mask the symptoms of Reye’s Syndrome or increase it’s severity.
By two o’clock on Saturday afternoon, Julie’s condition was rapidly deteriorating. She became extremely restless, confused and disoriented. When she complained of “black spots in front of her eyes”, I ran to the telephone and called the doctor. He said he would meet me at Children’s Medical Center.
How could I get there? Could Leah’s mother stay with the children? Could I get Julie there alone? What if she dies on the way?
I struggled to get her out of bed and on her feet. She was so lethargic and didn’t want to get up. Somehow, I got her into the hallway. I looked up and there was her Dad coming toward us. He picked her up and put her into the back seat of the car. As we pulled away I glanced back at the house. Karen and Meghan were standing and waving on the front porch.
It was the last time they ever saw their big sister alive.
On that hot Saturday afternoon, confusion reigned at the Children’s Medical Center. There had been a rash of admissions to the emergency room and it was more than two hours before Dr. C. was advised that his patient was there.
During that time Julie became more incoherent and couldn’t even tell me her name. A young resident shocked me when he asked if she might have somehow obtained “drugs”. Julie was thrashing about in the bed and was so uncooperative that the nurse had to restrain her to draw blood and start an IV infusion. Her behavior was so uncharacteristic of the little girl we knew and loved. At one point she even bit my hand.
I remember that suddenly Dr. C. appeared at the foot of her bed. He said nothing, turned away and left the room.
It was no more than ten minutes before Dr. C. returned accompanied by another doctor dressed in casual clothes. He introduced us to Dr. Steve, a specialist in gastroenterology, who recently came from Emory University Hospital in Atlanta.
He quickly examined Julie and asked if I had given her aspirin. Confused by the question I answered, “Not since last Monday…for her sore throat and fever”. He then said that he had the results of the blood work and she had Reye’s Syndrome.
I backed away…so stunned by those words he might as well have hit me with a baseball bat. The illness I knew killed a number of children in Michigan two years ago. The illness that is so rare I believed it could never happen to one of my children. Aspirin? ASPIRIN? What did aspirin have to do with it? Terrified, I watched as they rushed her to ICU.
Time stood still. It was an eternity before Dr. Steve came out to the waiting room. He was cautiously optimistic and explained that she was in Stage II… but was not in coma.
She was receiving mannitol, a drug to reduce the swelling in her brain and carefully regulated IV fluids to keep her hydrated. At present he did not feel it necessary to insert an intracranial pressure monitor.
The nurse told us that we could not stay with her as she might become more agitated. We could visit for ten minutes on the hour, every hour.
But she must be frightened. I wanted to see her, comfort her, love her. How could I possibly “agitate” her?
We waited…each interminable hour.
At five o’clock on Sunday morning, August 3rd, my restless sleep was disturbed by a clap of thunder. I hurried to the intercom and asked to see Julie.
When I entered the unit I was devastated by what I saw and heard…a rasping sound from her throat…large, fixed and dilated pupils…decerebrate rigidity. The nurse was across the room. I called to her for help.
On Monday, August 4, at 6:00 P.M., one week after the onset of a mild viral infection, Julie was removed from life support.
In the twenty minutes that her heart remained beating, I placed my hand in the palm of her hand. I told her that when I let go, her grandmother would be there to show her the way to God.
And He would forever hold her in the palm of His hand.
