FDA Statement: “Aside from drugs for fever or pain, most over-the-counter products haven’t actually been studied in children for effectiveness, safety, or dosing.”
In a recent poll conducted by University of Michigan C.S. Mott Children’s Hospital, 40 percent of parents are giving  children under the age of 4 over the counter cold medicines, even after the FDA issued a warning that OTC medicines should not be used in this age group. Twenty Five percent of these parents gave their child decongestants!
children under the age of 4 over the counter cold medicines, even after the FDA issued a warning that OTC medicines should not be used in this age group. Twenty Five percent of these parents gave their child decongestants!
Manufacturers of OTC cold medicines changed their warning labels in 2008 to reflect the dangers of giving these medicines to young children, Six years of age and under.
One of the problems is that the medicines themselves are still labeled “Children’s” medication, and just like the issue with “Baby” aspirin, parents don’t think to read the label and they assume the product is safe for all children when in fact, it is not.
(Currently, there is no longer a product packaged or marketed as “baby aspirin” because in 2011, the National Reye’s Syndrome Foundation met with the FDA, stressing the danger in using the term “baby” in representing low-dose aspirin. FDA and aspirin manufacturers agreed, and there is no such thing as ‘baby’ aspirin anymore, and children are safer because of this change.)
The side effects from use of cough and cold medicines in young children may include:
- allergic reactions
- increased or uneven heart rate
- drowsiness or sleeplessness
- slow and shallow breathing
- confusion or hallucinations
- convulsions
- nausea
- constipation.
“Products like these may work for adults, and parents think it could help their children as well. But what’s good for adults is not always good for children,” says Dr Matthew Davis, Director of the C.S. Mott Children’s Hospital National Poll on Children’s Health.
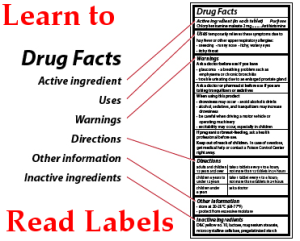
OTC drugs have information on the bottle or box. Always read this information before using the medicine. This information tells you:
How much to give; Medication doses for infants and young children are based on age and weight. Know your child’s weight.
Follow the directions for age and weight. If the recommended age is not your child’s age, don’t give the medicine.
If no dose is given on the bottle or package for children under 12 years old, ask your doctor or pharmacist if it is OK to give the medicine to your child, how much you should give, and when you should give it.
Liquid medicines usually come with a cup, spoon or syringe to help measure the right dose. Always use these devices to give medicine to infants and very young children. Using a kitchen teaspoon is not an accurate way to measure. A teaspoon is usually considered to be 5 cc or 5 mL, but kitchen teaspoons can vary in size from between 2 mL and 10 mL.
If you want to mix medicine with milk or formula, first put the medicine in one ounce of milk and have the child drink it all. Then feed the remaining formula or milk in the bottle and let them finish however much more they want.
Always measure or give medication with a good light turned on. Insufficient light could cause you to give the wrong medicine or the wrong dose.
Never let young children take medicine by themselves.
How often to give Medicines; Some medicines state every 6 hours, or every 8 hours. Does this mean ‘waking’ hours; hours when the child is awake, or actual hours as around the clock? Ask your Pharmacist this question so you know exactly when to give your child the medicine. Then keep track of the times you give the medicine to your child on a chart tapped to your refridgerator, or the location the medication is stored.
What the drug contains – Be certain you are not double dosing your child!
Many OTC cough and cold medicines contain a combination of ingredients to treat several symptoms. Your child might be getting some of the same ingredients in other medicines. For example, Tylenol and Nyquil contain the same ingredient, acetaminophen. Be sure to read the list of active ingredients (the ingredients that make the medicine work) for each OTC medicine you give your child to make sure he or she is not getting a double dose of the same medication. You need to make sure that the total amount of a medicine does not exceed the recommended dose.
Combinations of medicines found in multi-symptom medicines may cause side effects in children. The combination of antihistamines and decongestants in some “cold remedy” medicines can have side effects such as hyperactivity, sleeplessness and irritability in children. To be safe, don’t combine prescriptions, supplements or multi-symptom medicines without checking with your health care provider or pharmacist.
Watch The Ingredients List:
Sometimes the ingredients for a medicine change but the name stays the same. For example, the formulation of Kaopectate, an OTC medicine for diarrhea, changed so it now contains bismuth subsalicylate. The older versions contained only kaolin and pectin. (Bismuth subsalicylate is also found in Pepto-Bismol, an OTC medicine for upset stomach and diarrhea.) Bismuth subsalicylate is NOT recommended for children younger than 19 because of the risk of the rare but deadly condition; Reye’s Syndrome.
Because of Reye’s syndrome, DO NOT give a child younger than 19 any product with aspirin or similar drugs called “salicylates” unless your doctor tells you to. Instead of aspirin or other salicylates, you can give your child acetaminophen (sold as Tylenol and other brands). There are many names for aspirin (salicylates) and you can see the list here: https://reyessyndrome.wordpress.com/2012/12/30/other-names-for-aspirin/
Be sure to take into consideration the concentrations of ingredients when you determine the amount you give your child. Medicines with the same brand name can be sold in different strengths, including infant, children and adult formulas. Infant drops of some medicines, for example, are stronger than the liquid elixir of the same medicine for toddlers or children. This is because infants may not be able to drink a large volume of medicine to give their proper dosage. Don’t make the mistake of giving higher doses of the infant drops to a toddler thinking the drops are not as strong.
Warnings about using the drug: Always Read the ‘Black Box’ – the warnings box!
If the drug is safe for children of certain ages: If your child’s age is not listed, do not use the product. One exception to age, is the Reye’s Syndrome warning on labels: The National Reye’s Syndrome Foundation collects Case Reports of Reye’s Syndrome and has found that Reye’s predominately attacks children up to the age of 19, whereas the FDA label only states age 12. Don’t use aspirin or aspirin containing products in children under the age of 19.
And if you are not sure – Ask the Pharmacist at the store. They will be happy to help you!
Other Tips:
Talk to your doctor, pharmacist, or nurse to find out what mixes well and what doesn’t. Medicines, vitamins, supplements, foods and beverages don’t always mix well with one another. Select products with the fewest number of ingredients needed to treat your symptoms.
Talk to your Doctor or Pharmacist before giving a child a ‘home remedy’, or homeopathic drug found on the Internet! Many of these are quite harmful, and have no professional approval to use. Know what you are giving your child, otherwise, it could be deadly!
Don’t call medications “candy.” If children come upon medications at a later time, they may consider it “candy” and eat it without your knowing.
Always use child-resistant caps and store medicines in a safe place. Relock the cap after each use. Be especially careful with any products that contain iron; they are the leading cause of poisoning deaths in young children. All medications become less effective (expire) over time and should be replaced. Check the expiration date before using any product.
Store medicines in a cool, dry area. The heat from kitchens and the moisture from bathrooms decrease the effectiveness of medications. Store all medications out of the reach of children.
Before you give a medicine, check the outside packaging for damage such as cuts, slices, or tears; check the label on the 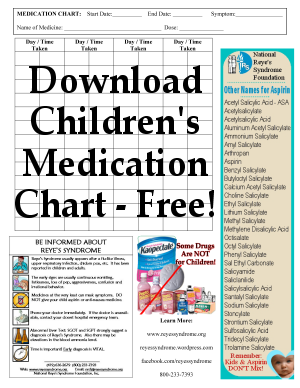 inside package to be sure you have the right medicine. Make sure the lid and seal are not broken. Check the color, shape, size and smell of the medicine. If you notice anything different or unusual, talk to a pharmacist or your health care provider.
inside package to be sure you have the right medicine. Make sure the lid and seal are not broken. Check the color, shape, size and smell of the medicine. If you notice anything different or unusual, talk to a pharmacist or your health care provider.
Use a chart to keep track of dosage dates and times. A Free Chart can be downloaded by clicking here.
Classes of OTC Medicines
Analgesics treat pain and fever:
Use caution with different forms of these drugs, because some are more concentrated than others. Common analgesics for infants and children are acetaminophen (Tylenol) and ibuprofen (Advil and Motrin).
WARNINGS:
- DO NOT give aspirin to children younger than 19, because it can cause a rare but deadly disease called Reye’s Syndrome.
- DO NOT use ibuprofen in children younger than 6 months. Know how much your child weighs before giving ibuprofen.
Antihistamines treat runny noses, itchy eyes and sneezing caused by allergies (but not colds). Some can cause sleepiness. Examples of antihistamines include brompheniramine (often in combination with decongestants such as phenylephrine as in Dimetapp and other medicines); chlorpheniramine (Chlor-Trimeton and other medicines); diphenhydramine (Benadryl and other medicines); cetrizine (Zyrtec); and loratadine (Claritin and other medicines).
WARNINGS:
- These are not recommended for children younger than 6, because they can even affect learning.
- Use only with your health care provider’s advice in young infants or children with asthma.
Expectorants and combination cough medications may help loosen mucus. Cough suppressants numb the reflex to cough. Coughing is necessary to clear mucus and debris bacteria from the lungs, so check with your child’s health care provider before using cough-suppressing syrups. Guaifenesin, an expectorant, promotes the production of thin mucus that is more easily removed by coughing.
WARNINGS:
- These are not recomended for children under the age of 6.
Decongestants can relieve stuffiness caused by allergies or colds by temporarily shrinking the membranes in the nose to make breathing easier. They should not be used for more than two to three consecutive days. Decongestants taken by mouth can have a number of side effects such as irritability, sleeplessness, dizziness. Examples of decongestants include phenylephrine (found in Neo-Synephrine nose drops and other medicines); and pseudoephedrine (Sudafed, PediaCare Infant Decongestant Drops and other medicines).
WARNINGS:
- These are not recommended for children under the age of 6.
Medicines for diarrhea. These are usually not necessary. Instead, give your child plenty of fluids and let the disease run its course. Diarrhea, however, can be dangerous in newborns and infants. In small children, severe diarrhea lasting just a day or two can lead to dehydration. Because a child can die from dehydration within a few days, you should see a health care provider as soon as possible if an infant has diarrhea. Talk to your provider before giving these medicines to infants or children.
WARNINGS:
- Diarrhea medicines containing bismuth subsalicylate (Pepto-Bismol, Kaopectate, and other medicines) should NOT be given to a child younger than 19, as these could trigger Reye’s Syndrome, a deadly disease in children.
- Loperamide (Imodium and other medicines), should NOT be given to a child younger than 6.
Laxatives relieve constipation and work by several methods. Some add fiber or water to stool to make it more bulky and easier for intestines to eliminate it; some coat the surface of the stool to make it more slippery; some soften the stool so it passes more easily; and others cause the intestines to contract more forcefully. Examples of laxatives include glycerin suppositories; magnesium citrate; magnesium hydroxide (Milk of Magnesia and other medicines); mineral oil (Agoral, Kondremul and other medicines); psyllium (Metamucil, Fiberall and other medicines); senna (Senokot, Ex-Lax and other medicines); methylcellulose (Citrucel and others), castor oil, and sodium phosphate (Fleet and other medicines).
WARNINGS:
- DO NOT give infants or children laxatives without talking to your child’s health care provider.
Summary:
Aside from drugs for fever or pain, most over-the-counter products haven’t actually been studied in children for effectiveness, safety, or dosing.
- When you give medicine to your child, be sure you’re giving the right medicine and the right amount.
- Read and follow the label directions.
- Use the correct dosing device. If the label says two teaspoons and you’re using a dosing cup with ounces only, don’t guess. Get the proper measuring device. Don’t substitute another item, such as a kitchen spoon.
- Talk to your doctor, pharmacist, or other health care provider before giving two medicines at the same time. That way, you can avoid a possible overdose or an unwanted interaction.
- Follow age and weight limit recommendations. If the label says don’t give to children under a certain age or weight, don’t do it.
Resources:
National Reye’s Syndrome Foundation, Food and Drug Administration, CDC, National Institutes of Health
Related Information:
What Is Reye’s Syndrome
Aspirin and Reye’s Syndrome
Other Names for Aspirin
Teens & Aspirin
Chicken Pox Parties
Herbal Remedies
Like this information?